- Over 55,000 LASIK and cataract procedures (including on over 4,000 doctors)
- The FIRST center in TN to offer Laser Cataract Surgery
- Introduced bladeless all-laser LASIK to the state
- Implanted the state's first FOREVER YOUNG™ Lens
- The first surgeons in the US to perform a new Intacs surgery to treat keratoconus
- Helped patients from 40 states and 55 countries
- International referral center for cataract surgery and LASIK complications
- Read Dr. Wang's book: LASIK Vision Correction
Why did you decide to have LASIK? Why did you choose Dr. Wang? How has your life changed since your LASIK procedure?
What is your advice for people considering LASIK?
Click to read more
| Home | Print This Page |
Contraindications to Implantation of Toric IOLs
Lance J. Kugler, MD, Dora Sztipanovits, OD, MS, Ming Wang, MD, PhD
Refractive Eyecare March 2011
Toric IOLs are an excellent technology for the correction of residual astigmatism following cataract surgery, but there are some patients for whom toric IOLs may be unsuitable.
Toric intraocular lenses (IOLs) are gaining popularity among cataract surgeons because they can provide effective correction of residual corneal astigmatism. Compared to other types of premium IOLs, including multifocal and accommodating, the results with toric IOLs are typically more predictable, and patient satisfaction is high.
As with any new technology, however, there are limitations to toric IOLs—they are not an appropriate solution for every patient with corneal astigmatism. This article summarizes three known contraindications to toric IOLs, including eyes with significant irregular astigmatism, eyes with progressive corneal disease, and eyes in which the astigmatism cannot be measured reliably.
Significant Irregular Astigmatism
Currently available toric IOLs correct regular astigmatism but may not be helpful in eyes with coexisting irregular astigmatism. In eyes with frank or forme fruste keratoconus, for example, a significant portion of the astigmatism is irregular. Patients with irregular astigmatism tend to find a small area of the cornea through which they are able to focus most clearly, and it is difficult to determine the axis and magnitude of astigmatism through that small window. Not only is proper alignment of a toric IOL difficult to achieve in these eyes, but even with perfect alignment there will still be a significant amount of irregular astigmatism remaining; and this may induce higher order aberrations due to complex coupling of the IOL’s toricity with the corneal irregularity.
Patients who required a gas permeable (GP) contact lens for correction of irregular corneal astigmatism prior to cataract surgery will likely continue to need a GP lens to see well after surgery. Here is where toric IOL implantation can run into trouble: If there is a GP lens neutralizing the corneal astigmatism on an eye with an implanted toric IOL, the contact lens will unmask the astigmatism in the toric IOL, and a significant amount of astigmatism will be seen in the patient’s GP lens overrefraction. This is because a GP lens typically neutralizes all corneal astigmatism, regular and irregular, allowing the net toricity of the toric IOL to manifest itself in the patient’s refraction.
A front-surface toric GP lens may be used to neutralize both the corneal irregularity and the lenticular astigmatism arising from the toric IOL, but front-surface toric GP lenses are difficult to fit, particularly in eyes with keratoconus. It is very difficult to prevent rotation in front surface GP lenses; but even small amounts of toric contact lens rotation will cause improper alignment of the astigmatic axis and reduce vision.
Therefore, eyes that will require GP lenses after cataract surgery implantation will do better with a traditional monofocal IOL than with a toric IOL. With a monofocal IOL in place, a spherical GP lens remains a viable solution for neutralizing postoperative regular and irregular corneal astigmatism—without creating a complex optical system that would require fitting a front-surface toric GP lens.
Progressive Corneal Disease
The current generation of toric IOLs have been successful largely because of their stability within the capsular bag. No less important is the stability of the axis of the corneal astigmatism to which the IOL is aligned. In eyes with progressive corneal disease, such as keratoconus, keratoectasia, Salzmanns nodular degeneration, or Terriens marginal degeneration, the axis and magnitude of astigmatism is likely to change over the years. Thus, what once was a properly aligned and powered toric IOL may end up being misaligned. In such eyes, toric IOLs should be avoided.
Uncertain Measurements
The success of cataract surgery with implantation of a toric IOL depends heavily on the accurate determination of the axis and power of corneal astigmatism. Even with the multitude of precision instruments at our disposal—including manual and automated keratometers, corneal topographers, and corneal tomographers—there are conditions in which reliable and reproducible measurements of corneal astigmatism remain elusive.
In eyes with a disrupted tear film, such as occurs in dry eye disease—a condition highly prevalent in the cataract surgery population—instrument readings are less reliable, and the quality of corneal astigmatism data is reduced. In such instances, one may have to resort to manual keratometry since the quality of the mire images can help gauge the degree of corneal irregularity. Manual keratometry, however, is inherently susceptible to operator error and does not directly measure the curvature in the central cornea.
Prior keratorefractive surgery represents another increasingly encountered source of problematic eyes. Such eyes have optical zone profiles that differ from virgin eyes, and may also have areas of irregularity that can confuse automated keratometers. Unfortunately, manual keratometers are less useful as a gauge for the degree of corneal irregularity in post-refractive eyes; since in such eyes, manual keratometers cannot directly measure the central corneal curvature. In these eyes, toric IOLs may be contraindicated.
Case Study 1: Residual Corneal Astigmatism
Figure 1 shows the topography of the right eye of a 55-year-old male who presented for cataract surgery. He had worn GP contact lenses for 20 years because of dissatisfaction with visual acuity in soft lenses. Manifest refraction of the right eye was –5.00 +1.75 X 080, which gave a visual acuity of 20/80. Overrefraction with a GP lens improved acuity to 20/40. Keratometry measured 45.00 D X 47.00 D @ 76o, and was consistent when measured by automated keratometry, manual keratometry, and two topography systems. Topography findings are consistent with forme fruste keratoconus.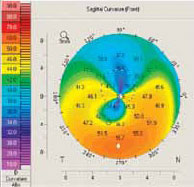
Calculations suggested using a toric IOL with 2.06 D of cylinder power at the corneal plane aligned at 82o. The danger in this case, however, is that this eye will likely require a GP lens postoperatively to neutralize the irregular astigmatism that is not correctable with the toric IOL. But the combination of toric IOL implantation and GP contact lens would result in refractive astigmatism of roughly +2.06 D @ 172o. Therefore, in this patient the more appropriate choice is a monofocal IOL teamed with a GP lens to neutralize the regular and irregular corneal astigmatism.
Case Study 2: Prior Refractive Surgery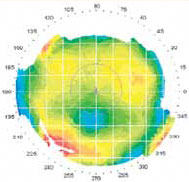
A 59-year-old woman with a history of PRK 15 years ago presented for cataract surgery of the left eye. Since her PRK she has worn glasses for night driving, but otherwise she has not worn correction. Manifest refraction was –0.75 +1.00 X 045. Automated keratometry measures 38.00 D X 38.50 D @ 85o. Manual keratometry measures 41.50 D X 43.00 D @ 100o. Corneal topography shows a decentered PRK ablation (Figure 2).
Although the patient’s vision was not adversely affected by the decentration, it caused the keratometry readings to be unreliable and inconsistent. Without reliable and consistent keratometry values, a toric IOL is not recommended.
The Bottom Line
Toric IOLs have become an increasingly popular means of reducing residual corneal astigmatism following cataract surgery. As good as it is, however, toric IOL technology has limitations and may be contraindicated in eyes with significant corneal irregularity due to keratoconus (frank or forme fruste). Eyes with progressive conditions that may affect the axis and power of corneal astigmatism (eg, Salzmanns nodular degeneration or Terriens marginal degeneration) are also poor candidates for toric IOLs. Finally, conditions such as dry eye disease or a history of prior corneal refractive surgery can make it difficult to obtain accurate measurements of corneal astigmatism. In these cases, it may be best to avoid toric IOLs.
Lance J. Kugler, MD, is in private practice at LaserVision Correction in Omaha, NE, and serves as the director of Refractive Surgery at the University of Nebraska Medical Center. Dora Sztipanovits, OD, MS, is an optometrist at the Wang Vision Cataract and Lasik Center, Nashville, TN. Ming Wang, MD, PhD, is a clinical associate professor of ophthalmology of the University of Tennessee, director of Wang Vision Cataract and Lasik Center, Nashville, TN.
Our new texbooks
A 501c(3) charity that has helped patients from over 40 states in the US and 55 countries, with all sight restoration surgeries performed free-of-charge.