- Over 55,000 LASIK and cataract procedures (including on over 4,000 doctors)
- The FIRST center in TN to offer Laser Cataract Surgery
- Introduced bladeless all-laser LASIK to the state
- Implanted the state's first FOREVER YOUNG™ Lens
- The first surgeons in the US to perform a new Intacs surgery to treat keratoconus
- Helped patients from 40 states and 55 countries
- International referral center for cataract surgery and LASIK complications
- Read Dr. Wang's book: LASIK Vision Correction
Why did you decide to have LASIK? Why did you choose Dr. Wang? How has your life changed since your LASIK procedure?
What is your advice for people considering LASIK?
Click to read more
| Home | Print This Page |
Surgeon describes best techniques to correct a decentered ablation
Ming Wang, MD, describes decentered ablations and the course of action needed to remedy them.
by Ming Wang, PhD, MD,Wang Vision 3D Cataract and LASIK Center, Nashville, Tennessee
Introduction
 |
Significantly decentered excimer ablations result in loss of best corrected visual acuity due to irregular astigmatism and cause symptoms such as glare, night vision difficulty, ghosting and diplopia. Possible causes of decentration include poor fixation due to poor patient instruction, anxiety, over-sedation, blurry vision due to high refractive error or the exposed stromal bed causing difficulty seeing the laser’s target. It can also be due to improper stabilization of the patient’s eye with a Thornton ring during ablation. In order to prevent decentration, careful preoperative and intraoperative instructions are key, especially with regard to the fixation target. My special guest in this column is Ming Wang, MD, to explain how to handle this complication. |
| Amar Agarwal | |
| Amar Agarwal, MS, FRCS, FRCOphth |
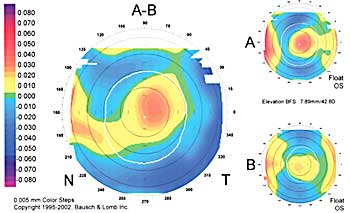
Dioptric curvature maps indicate surface shape using the axial radius of curvature, or the distance along the normal from the surface to the optic axis. Once a radius is determined, it is converted to a dioptric value using a paraxial keratometry formula. This value indicates the surface refractive power when incident rays are normal to the cornea; therefore, it is valid for the corneal apex only. When this formula is applied to all corneal points, radius-based dioptric maps misrepresent corneal power. Instead, radius-based dioptric maps should be thought of as dioptric curvature maps.
In contrast, elevation maps using an appropriate reference surface can describe subtle variations in surface geometry and are valuable when true topography is required. Elevation maps are useful in both diagnoses and treatment of decentration, and in monitoring surface changes.
Keratoconus presents a corneal condition resulting in progressive decentration of the corneal apex. On the axial map, keratoconus appears as an area of inferior steepening. On the elevation map, the cornea is elevated superior to the area of thinning.
The key observation on curvature maps is the dioptric difference between the superior and inferior keratometric readings. The key observation on elevation maps is the misalignment of the center of ablation from the optical center.
Typical case presentation
A patient with a decentered ablation generally presents with the following clinical signs and symptoms:
- A decentration of the ablation zone on corneal topography.
- Increased higher-order aberrations as measured using wavefront aberrometry, predominantly coma.
- The appearance of a tail on point spread function.
- Reduced best corrected visual acuity that improves only with gas permeable lenses.
- A cylinder measurement on autorefraction and wavefront that differs from manifest refraction.
- A history of reduced vision immediately after surgery that fails to improve with time.
Topographic decentration
To evaluate decentration on corneal topography, both axial curvature and elevation maps are useful. The axial algorithm provides the refractive result of ablation, ie, the optical zone. A large corneal curvature gradient between treated and untreated cornea, such as that resulting from a highly myopic correction, creates a smaller optical zone, increasing the refractive effect of the decentration. The elevation algorithm delineates the location and size of the ablation zone. Decentration of the ablation zone can be measured by comparing the distance between the center of the flattened zone and the center of the entrance pupil on preoperative and postoperative elevation maps using a difference map (Figure).
Wavefront aberrations
Wavefront aberrometry shows increased higher-order aberrations in patients post-LASIK, specifically those with decentered ablations. Subclinical decentrations less than 1 mm significantly increase wavefront aberrations, deteriorating the optical quality of the retinal image. On average, all Zernike coefficients increased postoperatively, with coma being the predominant high-order aberration. Decentrations as small as 0.2 mm increased wavefront aberrations. However, decentrations less than 0.5 mm have been considered clinically insignificant.
Management
Relieving patients of symptoms associated with decentration may be complex. The most frequently used method involves gas permeable lenses, which reshape the anterior cornea optically to restore visual quality. These fittings often require reverse geometry lenses or aspheric lenses to be successful. Most patients do not want to venture down the road that motivated them to first pursue refractive surgery.
Surgical options are limited. For mild degrees of decentration after PRK, a small (3 mm to 4 mm) diameter ablation at the edge of the original optical zone can serve to enlarge the optical zone in the pupillary axis. Another technique involves a series of three small-diameter ablations at the edge of the decentered ablation followed by phototherapeutic keratectomy smoothing. There is a risk of hyperopic shift due to the removal of tissue centrally. These two methods are difficult post-LASIK because the enhancement will be constrained by the size of the original bed.
Custom-Corneal Ablation Pattern (Custom-CAP, Visx) received U.S. Humanitarian Use Device approval for the treatment of decentrations in 2002. Elevation data is obtained using the Humphrey Atlas (Carl Zeiss Meditec), and a software program allows simulation of surgeon-directed ablations of chosen location, shape, size and depth to improve corneal topographic appearance. Although effective, Custom-CAP does not address the refractive error. While most surgeons consider an improvement in BCVA and reduction of symptoms a surgical success, many patients are frustrated by the lack of improvement or, in some cases, worsening of uncorrected vision.
Wavefront-driven custom treatment may be used to correct decentrations, assuming the technology currently available is able to detect the irregularities reliably. Shack-Hartmann aberrometers may fail when attempting to measure eyes with considerable irregularity, due to limitations of the lenslet array. While decentrations may increase higher-order aberrations, attempting to correct the aberrations may not fully correct the topographical errors. These systems assume a normal prolate cornea in treatment planning, and the refractive error corrections may be less accurate. Thus, these treatments may be less effective than topographically directed treatments.
Re-treatment using conventional enhancement techniques rarely fully corrects the problem and typically increases the effective decentration. This occurs because the neural axes (visual axis and line of sight) and the optical axis (geometrical) are not aligned in cases of decentration. Image placement on the fovea requires the eye to rotate, making full correction of the optical problem unlikely when all measurement and planning occurs on the visual axis. Conventional technology is not able to decouple these axes and treats solely on the visual axis information.
The advancement of Scheimpflug imaging to create three-dimensional models of corneal shape may be the missing link to accurate topographically driven treatments. These systems measure the corneal shape directly and with greater accuracy than placido or slit scanning methods. Combining precise topographical measurements with sophisticated software programs, such as the Corneal Integrated Planning and Treatment Algorithm (CIPTA, Ligi) software, may enable treatment of irregular astigmatism.
For More Information:
- Amar Agarwal, MS, FRCS, FRCOphth is director of Dr. Agarwal’s Group of Eye Hospitals. Dr. Agarwal is author of several books published by SLACK, Incorporated, publisher of Ocular Surgery News, including Phaco Nightmares: Conquering Cataract Catastrophes, Bimanual Phaco: Mastering the Phakonit/MICS Technique, Dry Eye: A Practical Guide to Ocular Surface Disorders and Stem Cell Surgery, and Presbyopia: A Surgical Textbook. He can be reached at 19 Cathedral Road, Chennai 600 086, India; fax: 91-44-28115871; e-mail: dragarwal@vsnl.com; Web site: www.dragarwal.com.
- Ming Wang, MD, PhD, can be reached at Wang Vision 3D Cataract and LASIK Center, 1801 W. End Ave., 11th Floor, Nashville, TN 37203; 615-321-8881; fax: 615-321-8874; e-mail: drwang@wangvisioninstitute.com.
References:
- Agarwal A. Handbook of Ophthalmology. Thorofare, NJ: SLACK Incorporated; 2005.
- Agarwal A. Refractive Surgery Nightmares. Thorofare, NJ: SLACK Incorporated; 2007
- Agarwal A, Agarwal A, Agarwal S. Four Volume Textbook of Ophthalmology. New Delhi, India: Jaypee Brothers; 2000.
Read more: Surgeon describes best techniques to correct a decentered ablation
Our new texbooks
A 501c(3) charity that has helped patients from over 40 states in the US and 55 countries, with all sight restoration surgeries performed free-of-charge.